pest control in hospital settings is fundamentally different from pest control in homes, offices, or even most commercial environments. Hospitals operate under a zero-tolerance framework, where even minimal pest activity is considered a serious risk. A single insect sighting, rodent trace, or overlooked nesting area can compromise patient safety, contaminate sterile zones, and trigger compliance issues during audits or inspections.
This article explains why pest control in hospital environments requires a higher standard of control, documentation, and planning. It covers infection and contamination risks, regulatory compliance and audit readiness, Integrated Pest Management (IPM) as the core approach, differences in pest control priorities across hospital zones, the role of hospital staff in early detection, and how pricing structures and long-term planning are typically explained transparently without focusing on individual cost figures.
Why hospitals operate under a zero-tolerance pest control framework
In most environments, pest activity is treated as a nuisance problem. In hospitals, it is treated as a safety and infection control issue. The presence of pests in healthcare facilities directly contradicts the core purpose of a hospital: protecting and restoring health.
Hospitals operate under a zero-tolerance framework because:
- Patients often have weakened immune systems
- Open wounds, invasive devices, and sterile procedures are common
- Food preparation and waste handling occur continuously
- Facilities operate 24/7 with constant human movement
- Any contamination event can have severe consequences
In pest control in hospital settings, the goal is not to reduce pest activity to an acceptable level, but to prevent it entirely through structured prevention and monitoring.
Pests as carriers of pathogens in healthcare environments
Pests are not just unwanted intruders; they are potential vectors of disease. Many common pests carry bacteria, viruses, fungi, and parasites that can be transferred to surfaces, equipment, food, and even directly to patients.
Examples of pathogen transmission risks include:
- Cockroaches carrying bacteria such as E. coli and Salmonella
- Rodents spreading pathogens through urine, droppings, and fur
- Flies transferring contaminants from waste areas to sterile zones
- Ants moving through contaminated and clean areas without detection
- Mold spores affecting air quality and respiratory health
In pest control in hospital operations, even pests that are often ignored in other settings can pose serious risks due to their ability to move unnoticed between contaminated and sensitive areas.
The danger of often-overlooked pest species in hospitals
When people think of hospital pest problems, they often imagine rodents or cockroaches. However, some of the most dangerous risks come from pests that are easily overlooked.
Examples include:
- Small ants entering IV lines, medical equipment, or wound dressings
- Stored-product insects in pharmacy or supply areas
- Drain flies breeding in floor drains and sinks
- Birds nesting near ventilation intakes
- Dust mites and mold affecting indoor air quality
Effective pest control in hospital environments requires attention to these less obvious threats, not just visible infestations.
Regulatory compliance and audit readiness
Hospitals are subject to strict regulations, accreditation standards, and routine audits. Pest control is often reviewed as part of infection control, facility management, and patient safety assessments.
Regulatory compliance typically requires:
- Documented pest control programs
- Scheduled inspections and monitoring
- Clear treatment protocols
- Incident reporting systems
- Corrective action records
Pest control in hospital facilities must be designed not only to control pests but also to demonstrate compliance through proper documentation and traceability.
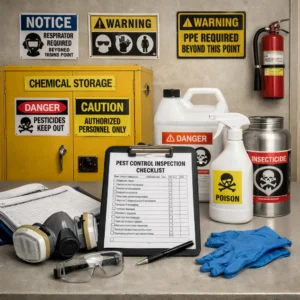
Documentation and monitoring systems
Documentation is a critical component of hospital pest control. It provides evidence that risks are being actively managed and that corrective actions are taken when issues arise.
Typical documentation includes:
- Inspection reports and findings
- Monitoring device logs
- Sighting records and response actions
- Treatment history and product usage
- Preventive recommendations and follow-ups
During audits, inspectors often review these records to verify that pest control in hospital environments is proactive rather than reactive.
Integrated Pest Management as the core approach
Integrated Pest Management (IPM) is the foundation of effective pest control in hospital settings. IPM focuses on prevention, monitoring, and control while minimizing reliance on chemical treatments.
The core principles of IPM include:
- Understanding pest biology and behavior
- Identifying risk factors and entry points
- Implementing exclusion and sanitation measures
- Monitoring pest activity continuously
- Using chemical treatments only when necessary
IPM allows hospitals to maintain pest-free environments while reducing exposure to chemicals in sensitive areas.
Non-chemical methods and exclusion strategies
In pest control in hospital environments, non-chemical methods are always prioritized. These methods reduce risk to patients, staff, and equipment.
Common non-chemical strategies include:
- Sealing gaps, cracks, and service penetrations
- Improving waste handling and storage practices
- Enhancing cleaning and sanitation protocols
- Installing physical barriers and screens
- Using monitoring traps instead of active pesticides
Chemical treatments are used only when monitoring confirms activity and when non-chemical controls are insufficient.
Minimizing chemical use in sensitive areas
Hospitals contain many sensitive zones where chemical use must be tightly controlled or avoided altogether. These include operating theaters, intensive care units, neonatal wards, and sterile storage areas.
Pest control in hospital settings addresses this by:
- Selecting low-toxicity and low-odor products when needed
- Applying treatments during controlled time windows
- Using targeted application methods
- Coordinating closely with hospital management
The goal is to eliminate pest risks without introducing new hazards.
Different risk profiles across hospital zones
Hospitals are complex facilities with zones that carry different pest risks and control priorities. A one-size-fits-all approach is ineffective.
Kitchens and food preparation areas
These areas attract pests due to food availability and waste. Control focuses on sanitation, exclusion, and frequent monitoring.
Patient rooms and wards
These areas require maximum safety and minimal disruption. Monitoring and preventive measures are prioritized, with chemical treatments used only when absolutely necessary.
Pharmacies and supply rooms
Stored-product pests and contamination risks are key concerns. Tight inventory control and monitoring are essential.
Loading docks and waste areas
These zones are high-risk entry points for pests. Pest control in hospital environments places strong emphasis on exclusion and external control in these areas.
The role of hospital staff in pest prevention
Pest control in hospital facilities is not the responsibility of external providers alone. Hospital staff play a critical role in early detection and prevention.
Staff involvement typically includes:
- Training to recognize early signs of pest activity
- Clear reporting protocols for sightings
- Understanding hygiene and waste management responsibilities
- Cooperation during inspections and treatments
Early reporting allows pest control teams to respond before issues escalate.
Shared responsibility and communication
Effective pest control in hospital environments relies on collaboration between facility management, healthcare staff, and pest control professionals.
Clear communication ensures:
- Timely response to reported issues
- Minimal disruption to hospital operations
- Alignment with infection control protocols
- Continuous improvement of preventive measures
Inspection processes and preventive planning
Regular inspections are a cornerstone of hospital pest control. Inspections identify risk factors before they result in infestations.
Preventive planning typically includes:
- Scheduled routine inspections
- Risk assessments for new or renovated areas
- Review of pest trends and monitoring data
- Adjustment of control strategies as needed
This proactive approach supports long-term control rather than emergency response.
Explaining pricing structure transparently
In pest control in hospital environments, pricing is usually explained based on scope, complexity, and ongoing requirements rather than individual treatments.
Pricing structures commonly reflect:
- Facility size and layout
- Risk level of different hospital zones
- Frequency of inspections and monitoring
- Documentation and reporting requirements
- Preventive and corrective measures
Transparent pricing ensures hospital management understands what services are included, how preventive planning is supported, and how long-term control is maintained.
Long-term pest control strategies for hospitals
Pest control in hospital facilities is an ongoing process, not a one-time service. Long-term strategies focus on prevention, monitoring, and continuous improvement.
Long-term control typically includes:
- Regular monitoring and reporting
- Preventive maintenance recommendations
- Staff awareness and training updates
- Review of pest control performance
Conclusion
Pest control in hospital environments operates under a zero-tolerance framework because patient safety, infection control, and regulatory compliance are at stake. By focusing on Integrated Pest Management, minimizing chemical use, maintaining detailed documentation, and involving hospital staff in early detection, healthcare facilities can manage pest risks responsibly. Long-term planning, transparent processes, and shared responsibility are essential to maintaining safe, compliant, and pest-free hospital environments.